Most processes in our body - whether to create molecules, breakdown molecules, or trigger the interaction of one molecule with another - involve the interaction of 1 or more protein molecules with another. This ‘interaction’ is determined to a large extent by the 3D structure of the interacting molecules. If one has a glove-like opening and the other a hand-like protrusion, there may be a fit and subsequent interaction. There are ennumerable 3D configurations in which these proteins exist (think of the countless unique lock-key combinations that exist). They may have different structures on different sides, allowing them to interact with more than 1 kind of counterpart molecule. They also may change configuration based on certain interactions. This variety of configurations and the ability to transform, allows a high degree of specificity in molecular interaction and is crucial for normal functioning of the body. A change in the structure of the molecule, can make it functionally abormal or even worthless. For instance, in sickle-cell anemia the structure of haemoglobin is different from normal, affecting its ability to bind oxygen molecules. Scientists use X-ray crystallography to understand the 3D structure of proteins and other molecules.
If you want a quick, beautiful primer on the human immune system, this Kurzgesagt video is amazing:
The first point of contact for any foreign organism entering the body will be a host of macrophages that will try to kill and/or ingest the offender. If this response is not sufficient to snuff out the infection, dendritic cells come into play. Dendritic cells:
recognize molecules on the surface of the offending organism,
alter their own surface by incorporating fragments of the organism (this fragment is called an ‘antigen’)
go searching for the ‘right’ T-cell that can neutralize the specific organism by recognizing the antigen present on the surface of the dendritic cell.
As such, Dendritic cells are also called ‘Antigen Presenting Cells’ (APCs) - they process the antigen from the offender and present it on their own surface for the T-cells to identify.
Note: There are also other cells such as Macrophages and B-lymphocytes that act as antigen-presenting cells. However, Dendritic cells are 10-100 times more potent in inducing T-cell proliferation1.
Dendritic cells are the "sentinel cells" of the mammalian immune system. Named after the Greek word for tree, they develop distinctive probing branches when activated, sweeping their environment in search of unwelcome things - like bacteria, viruses, tumours.
When dendritic cells encounter something they don't like, they take a physical marker of the invader, called an antigen, and present it to B and T cells, the defenders of the body' s immune system. Those cells then adapt weapons to identify and destroy the interlopers.
Steinman bet that if he could train his dendritic cells to recognise and tag his cancer, they would be able to convince the T and B cells to do the rest.
Nobel winner Ralph Steinman's quest to cure cancer - including his own, BBC
Dendritic cells are commonly found in areas of the body that are exposed to the outside environment - such as skin, the respiratory tract (lungs, trachea), digestive tract (stomach, oesophagus).
Why present antigens to T-cells?
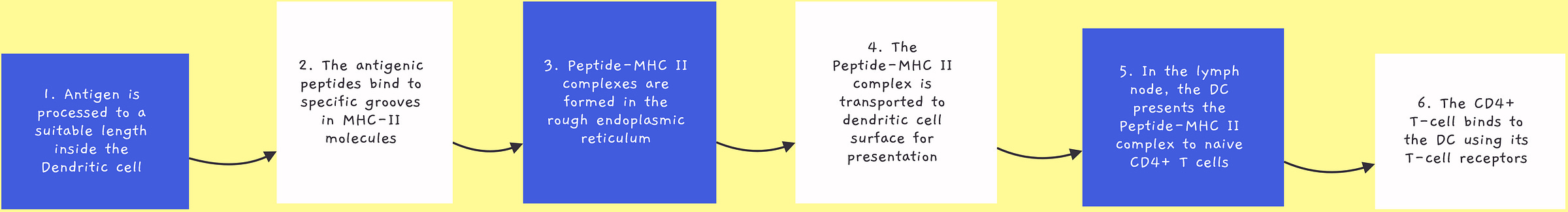
Present inside our spleen and bone marrow is a repository of T-cells known as memory T-cells. They literally serve as memory - each T-cell can recognize a specific antigen (identifying molecule). Dendritic cells carry antigens to this repository to find a T-cell that can identify and match with the specific antigen they’re carrying. The T-cell then binds to the Dendritic cell forming what is known as an “Immunological Synapse” imvolving many molecules on the Dendritic cell and T-cell surfaces. Other signalling molecules - all different proteins - are also required for the T-cell to become activated. The T-cell then makes many million copies of itself, all of which can recognize the specific antigen that it was presented. This population of T-cells then moves to the site of infection and begins eliminating the pathogen, with assistance from other immune cells and protein molecules.
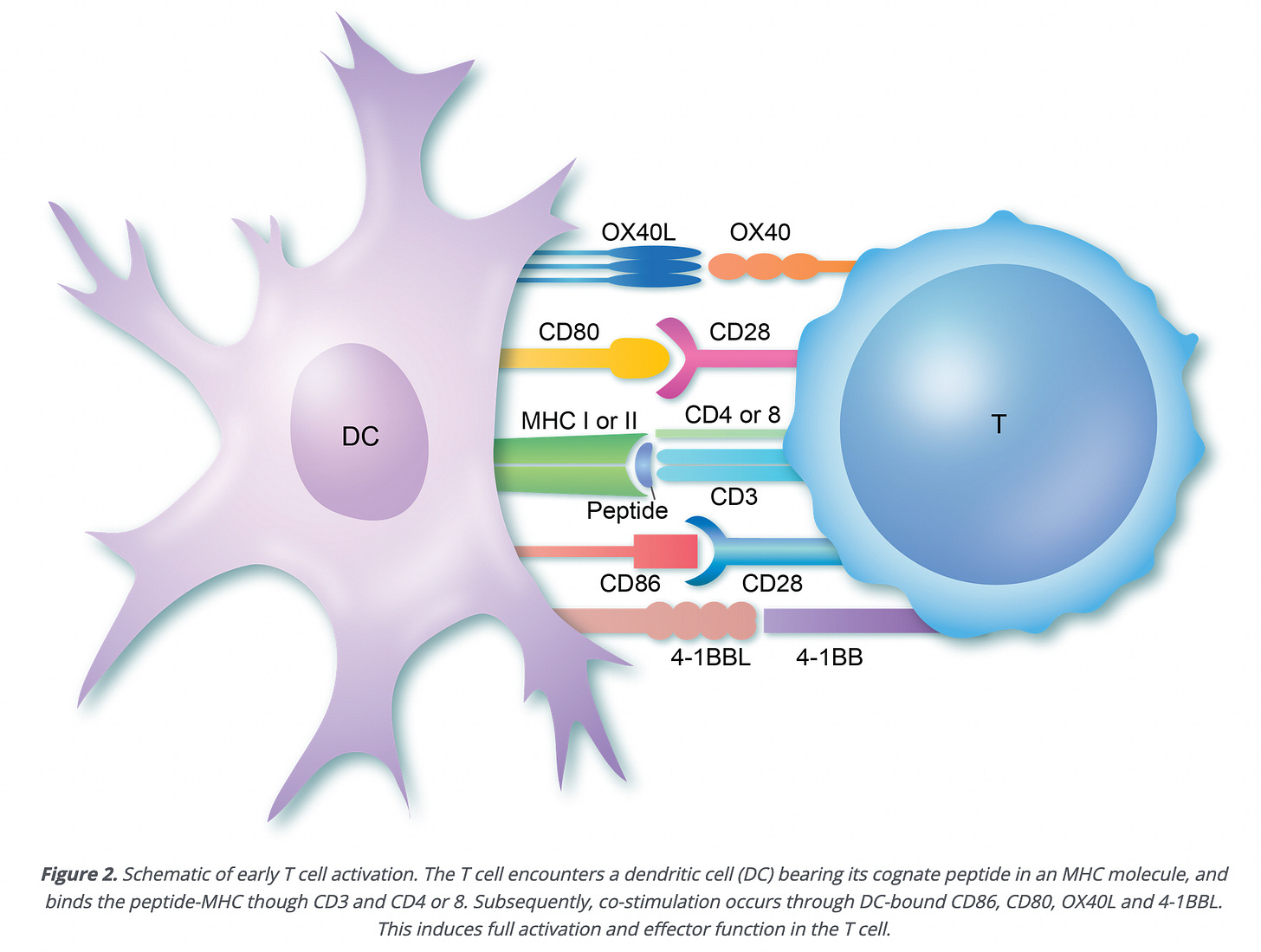
The ‘peptide’ on the MHC I or II molecule in the image above is the antigen we’ve been talking about. It’s a section of a protein taken from the pathogen that the body wants to kill. The ‘CD4 or 8’ is also a specific kind of protein that is found on T-cell surface. T-cells with CD4 are ‘helper T-cells’ (also called Th cells). T-cells with CD8 are ‘cytotoxic T cells’ (also called CTLs).
Dendritic Cell Vaccines for Cancer Immunotherapy
Dr. Ralph Steinman, 2011 Nobel Laureate in Medicine, is credited for the discovery of dendritic cells. Dr. Steinman was diagnosed with Pancreatic cancer in 2007 and was told he only had a few months to live. He collaborated with other reasearchers working in the field to test his ideas regarding dendritic-cell based immunotherapy and himself enrolled in clinical trials.
Cancer cells are ‘mutant’ body cells. They’re like any other cells in the body, but have developed means to escape the natural checks that exist, and are able to multiply rapidly and uncontrollably using up the resources of the body and making it difficult for normal cells to survive and carry out their functions. Treating cancer is a challenge because therapies such as chemotherapy (i.e. using drugs) affect not just cancer cells, but healthy body cells too. Dendritic cell vaccines offer the important possibility of triggering an immune response that can specifically target cancer cells, not attacking healthy cells. Dr. Steinman explains how in this video:
When diagnosed, Dr. Steinman was told he had only a few months to live, however he breathed his last in 2011, nearly 4 years after the diagnosis. Several studies have since been carried out to study the effect of dendritic cell based vaccines in cancer patients.
In clinical trials, cancer patients that received dendritic cell based vaccines in addition to chemotherapy showed better remission rates than those that received only chemotherapy. Another aspect that makes dendritic cell vaccines particularly useful is the ability to create ‘personalized vaccines’. Dendritic cells can be loaded with identifying molecules/structures from cancer cells taken from the patient, allowing highly specific immune responses.
Ultimately, these studies have all served to prove and extend Ralph’s original premise that dendritic cells are the cells vital for initiating the cellular immune response, for not only providing the antigen to resting T cells but for instructing the T cells to respond, and for influencing the quality as well as the magnitude of the response. From this, the principles of modern vaccinology have evolved, including the current focus on strategies to deliver the desired antigen to dendritic cells and promote maturation of the dendritic cell to efficiently induce the desired response.
Clinical trials with dendritic cell vaccines have shown improved survival rates in patients with stage III/IV melanoma (skin cancer). For glioblastoma, which is extremely hard to treat and has a very high fatality rate, after the cancer returns median life expectancy period is about ~6 months. In a trial with DC vaccines, median life expectancy was ~23 months in patients who underwent surgery and DC vaccination.
Dendritic Cell Vaccines are not yet ready for large scale use
Cancer cells develop ways to escape being hunted by immune cells in the body. This is carried out through “immunosuppressive factors” - molecules that play a role in modifying immune response. The presence of such molecules can reduce the effectiveness of dendritic cell vaccines.
Another challenge is ‘undesired immune response’. Think of autoimmune diseases such as rheumatoid arthritis, where immune cells inadvertently kill healthy cells in joints. Inducing immune response in the human body is tricky due to the number of different types of cells and proteins involved and an imperfect understanding of how all of them interact - we keep finding new information about the immune system. In this scenario, the occasional patient may have immune responses different from what was intended through giving them the dendritic cell vaccine.
There are also more specific challenges to using dendritic cell vaccines
Activation state of the DC - The effectiveness of dendritic cells in presenting antigens to T-cells and evoking an immune response also depends on the ‘lineage’ of the dendritic cell. There are many kinds of Dendritic cells based on which cell they originated from and which molecules were involved in their ‘maturation’. Some kinds, such as those derived from monocytes, are easier to isolate from patients and able to take up antigen and travel to lymph nodes for antigen presentation. They are more useful for dendritic cell vaccines than other kinds.
Selection of antigens that will activate both CD8+ and CD4+ T-cells in a potent, immune-specific manner - As discussed earlier, the T-cells with CD8 molecules are cytotoxic, whereas those with CD4 are the helper T-cells. Early dendritic cell vaccine trials where vaccines were focused on activating CD8+ T-cells alone had poorer results. CD4+ T helper cells have been shown to have antitumor activity through a variety of mechanisms. They’re also important for generation of memory T-cells (specifically ‘cytotoxic’ T-cells - they can kill the cells they recognize) and vaccines that are able to activate both CD8+ and CD4+ T helper cells may be more effective.
The antigen chosen for the DC vaccine should meet 4 basic criteria2:
“they should be specific to cancer, preferably mutated in the cancer of interest to increase immunogenicity and minimally expressed on normal tissues to avoid autoimmunity” - if the antigen is expressed on healthy body cells the immune response may damage normal body cells too. This criteria is hard to meet - the most promising antigen (the one that will be recognized and bound better) in a tumor cell may often be part of a protein produced in normal cells (called a ‘self protein’) which is produced in much larger quantities in a tumor cell. This is seen in breast cancer, with the HER2 protein.
“common in the cancer of interest” - the antigen should appear on the tumor cells in most (if not all) patients suffering from the specific kind of cancer
“play a role in tumor progression or survival” - the
“be capable of eliciting an antigen-specific immune response” - not all molecules/components of a foreign organism or a tumor cell are antigens
Effectiveness in patients with advanced stages of cancer - in these patients, the immune system has already weakened significantly and the immune response from a dendritic cell vaccine may not be sufficient to fight the cancer. Dendritic cell vaccines may be more effective in early stage cancer patients.
A number of biotech firms are focusing on developing dendritic cell based vaccines for cancer and other diseases. Being able to personalize the vaccines, as well as the possiblity of generating the immune response without having to extract dendritic cells and re-inject them into the patient, make them an exciting area of research.
References:
Article - Dr. Ralph Steinman: The Nobel Prize Winning Scientist who Became his own Patient
Article - Nobel winner Ralph Steinman's quest to cure cancer - including his own, BBC
Article - T-cell Activation, British Society of Immunology
Journal Article - Ralph M. Steinman: A man, a microscope, a cell, and so much more
Journal Article - The fabulous legacy of a Nobel Prize Laureate
Journal Article - Research progress on dendritic cell vaccines in cancer immunotherapy
Cintolo JA, Datta J, Mathew SJ, Czerniecki BJ. Dendritic cell-based vaccines: barriers and opportunities. Future Oncol. 2012 Oct;8(10):1273-99. doi: 10.2217/fon.12.125. PMID: 23130928; PMCID: PMC4260651.
Tai Y, Wang Q, Korner H, Zhang L, Wei W. Molecular Mechanisms of T Cells Activation by Dendritic Cells in Autoimmune Diseases. Front Pharmacol. 2018 Jun 26;9:642. doi: 10.3389/fphar.2018.00642. PMID: 29997500; PMCID: PMC6028573.
Video - Antigen Presenting Cells (Macrophages, Dendritic Cells and B-cells)
Video - Ralph Steinman, Nobel prize winner, speaks about dendritic cells and immune-based vaccines
Disclaimer:
All writing on Floating Coordinates and any online forum/website I use is for my own understanding of the topics I write about. I’m not a medical professional and do not provide medical advice in any manner. My writing will not be 100% scientifically accurate since I aim to explain simply and with as less jargon as possible. I welcome your comments to improve upon what I publish, however, this blog will not approach the specificity or accuracy of scientific publications.



